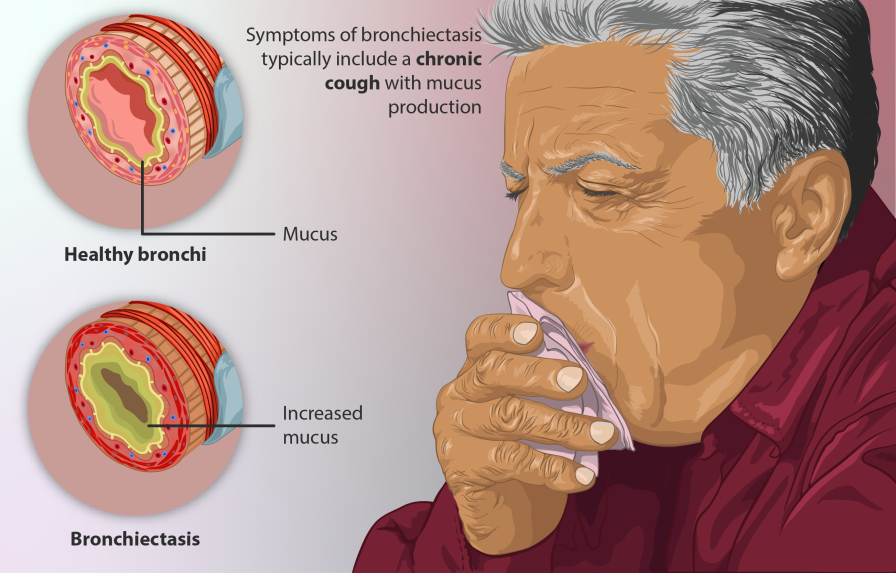
Are you coughing large amounts of mucus coughed up daily and are you feeling extremely tired? Are you observing thickening of the skin under your nails, chest pain, persistent cough, shortness of breath, and wheezing? Are you trying hard but not gaining weight? Your worry begins to increase and mind starts to race. Chances are you might be suffering from a lung condition “ Bronchiectasis”.
Bronchiectasis
Bronchiectasis is a type of lung condition where the lung tubes becomes damaged and permanently widened that leads to an accumulation of mucus in the lungs increasing risk of respiratory infection. You are likely to have symptoms of chesty cough, shortness of breath, tiredness, chronic sinusitis, chest discomfort and coughing up blood. Controlling bronchiectasis and avoiding major effects requires early identification and treatment.
Bronchiectasis risk increases with age, however younger individuals can also get the condition It is more common in women than men, and in boys than in girls. It is uncommon for bronchiectasis to be present at birth. Bronchiectasis can result in major health complications, including breathing difficulties, lung infections, and even death. You may be more likely to get bronchiectasis if you have cystic fibrosis, any lung disease that is long-lasting and irritable, severe or persistent lung infections, such as TB, nontuberculous mycobacteria (NTM), or pneumonia. You might not have an efficient immune system to tackle the diseases.
The origin of bronchiectasis that is not caused by cystic fibrosis is not usually identified. This is called bronchiectasis for no known reason. But in other cases, the grounds are:
- A severe lung infection in the past has hurt the lungs.
- Primary ciliary dyskinesia and alpha-1 antitrypsin deficiency are two genetic diseases.
- Immune system abnormalities that make fighting infections harder Breathing in fluids, food, or stomach acid into the lungs
- Aspergillosis is a fungal allergy that affects the lungs and airways.
- Other health problems, such as rheumatoid arthritis, Crohn’s disease, and Sjogren’s syndrome, are also common.
- Blocked passageways (airways that have been obstructed by something like a tumour or an inhaled item).
How does your doctor figure out if you have bronchiectasis?
People think that bronchiectasis is not diagnosed enough. If your symptoms make your doctor think you might have this disease, they are likely to recommend diagnostics like X-rays or CT scans of the chest that can show how healthy the lungs structures and tissues perform.
Blood tests and sputum cultures are done to determine if there are infections.
Lung function test can also be helpful for Bronchiectasis because it will tell you lungs are working with normal volumes and capacity for its optimal function of gases exchange between tissues matching your body’s oxygen requirements.
Bronchoscopy lets doctors look into the lungs. A light and a camera are attached to a tube that is put into the nose or mouth and then down the trachea into the lungs. Lung secretions can also be taken with this method. A bronchoscopy can also find and remove the object causing the blockage in cases where the airways are blocked.
Is bronchiectasis similar to bronchitis or emphysema
Bronchiectasis refers to the lung condition with dilatation of your bronchioles, the end part of your air tube(bronchi) that connects to your air sac. This leads to constant mucus secretion and accumulation leading to respiratory infections.
Bronchitis refers to lung condition with inflammation of the main bronchi tube leading to excess mucus secretion and constant irritation to lung tubes, the bronchus. But there is no issues of mucus plugging at the bronchioles level.
Emphysema refers to lung condition with inflammation of air sacs leading to failure of appropriate gas exchange resulting in less oxygen and more carbon dioxide in body tissues .
What should patients expect as a management plan for bronchiectasis?
Bronchiectasis is not curable, but it can be controlled. Treatment for bronchiectasis often requires a combination of medication and lifestyle changes. Your doctor might tell you to take medicine, use specific devices. Bronchiectasis treatment is also different depending on what stage you are in. There are things you do every day (called maintenance) and things you do when you have an exacerbation (worsening). If bronchiectasis is caused by a disease like an aspergillosis or a problem with the immune system, then that disease must be treated first. In some instances, surgery may be required.
Medical Management:
- Antibiotics are medicines used to treat infections caused by bacteria. These include pills and sprays that you breathe in (breathed in using a nebulizer machine).
- Macrolides are medicines that are used to treat both infections and inflammations.
- Some medicines change mucus and help you cough it up.
Respiratory Physiotherapy Management is essential to keep the bronchial hygiene:
- Airway clearance : Clearance of mucus( sputum) from the lungs is very crucial and can reduce the number of infections and reduce your cough.
- Active cycle of breathing techniques to do daily at home. They include:
Deep breathing – taking a long, slow, deep breath in through your nose if possible, holding your breath for 2 to 3 seconds, and breathing out gently, like a sigh
Breathing control – breathing gently, through your nose if possible. Keep your shoulders relaxed.
Huffing and coughing –This airway clearance technique are most effective before and after your HFCWO therapy to effectively clear mucus from the airways.
- Use of mucus-clearing devices help break up mucus and get it out of your airways.
e.g Positive expiratory pressure (PEP) devices you can hold in your hands e.g Power breathe or Acapella
- Chest clapping help to move mucus out of the body.
- Respiratory vest or vest therapy. The frequent oscillations help loosen mucus, propelling it toward your larger airways, where it’s easier to cough out.
Integrated care-: Pulmonary rehabilitation is a lung- body- mind conditioning programme to enable the conservative management of bronchiectasis and improve your quality of life.
- Social support is a very important factor while you are suffering from bronchiectasis. Studies show that higher levels of social support are associated with better self-care behavior in bronchiectasis. Studies found that functional social support from family members helped participants manage their disease. Having a caregiver is associated with higher levels of physical activity and greater participation in pulmonary rehabilitation in patients with bronchiectasis. Different research findings strengthen the critical significance of the social environment in affecting patients’ success with self-care. Higher social support is related to an improved quality of life and performance in adulthood bronchiectasis.
- Mental Health illnesses, such as anxiety and depression, affect a considerable proportion of patients with bronchiectasis. Increased incidences of anxiety and depression have been shown in patients with bronchiectasis. Management and assessment are essential in bronchiectasis as high levels of anxiety and depression are linked with poorer health-related quality of life.
How can you prevent bronchiectasis?
There is no way to stop bronchiectasis from happening at birth. But there are ways to keep from getting the damage to your lungs that causes bronchiectasis. Remember to maintain a bronchial hygiene routines, physical activity, healthy eating, sleep routines and adherence to medication regimens.
The prognosis for bronchiectasis has improved in recent years, much still depending on the individual case. Factors such as age, general health, and the frequency and severity of exacerbations all play a role in determining outlook. With proper treatment, however, many people with bronchiectasis can live relatively everyday lives. If you or someone you know has bronchiectasis, it is crucial to get treatment immediately to increase the likelihood of a favorable result.
The first step for reaching out for support. Reach our for integrated care support – Pulmonary rehabilitation and mental health.…….